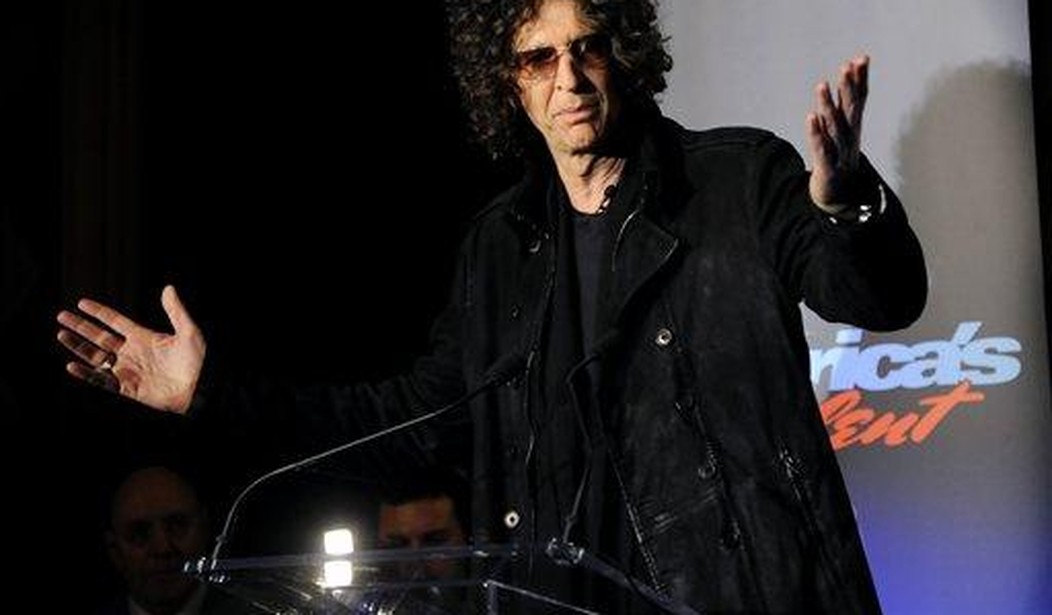
Hard pass on this idea, assuming it’s an earnest idea at all and not just a shock jock filling airtime.
.@HowardStern to a caller: “Americans don’t want to create a vaccine that’s going to turn you into a robot and magnetize you … Now, if you don’t get it, in my America, all hospitals would be closed to you. You’re gonna go home and die.” pic.twitter.com/WzWhiPmzp5
— The Recount (@therecount) January 20, 2022
I think it’s fine to consider vaccination status when deciding who gets a hospital bed if there aren’t enough beds to go around and if that status is just one factor in determining priority, not the deciding factor. It’s hard to argue that an unvaccinated 25-year-old should wait while a vaccinated 95-year-old with advanced cancer cuts the line.
If you want to incentivize the unvaxxed to get their shots, either jack up their insurance premiums or encourage their employers to lay down a mandate for staff. Handing them a bottle of ivermectin and turning them away at the ER when they’re desperately sick is punishment, not pressure, and it comes at a potentially high cost in deaths.
And America has had more than enough deaths, with another 50,000 to 300,000 to come by spring if the models are accurate. The higher end of that estimate would put us over a million fatalities at around the two-year anniversary of COVID arriving in the U.S.
Ed Yong tried to explain today to the Howard Stern wing of America’s vaccinated population that denying medical care to the unvaccinated is a terrible idea for many reasons:
People whose actions endangered themselves, like smokers with lung cancer or drivers who crash while not wearing a seatbelt, still get treated. Those whose actions endangered others, like drunk drivers or terrorists, also get treated. “We are all sinners,” Carla Keirns, a professor of medical ethics and palliative medicine at the University of Kansas Medical Center, told me. “No one has made all the perfect decisions, and any of us could find ourselves in a situation where we are sick.” It is a fundamental principle of modern medicine that “everyone has an equal claim to relief from suffering, no matter what they’ve done or haven’t done,” Daniel Goldberg, a medical historian and public-health ethicist at the University of Colorado, told me.
Moral arguments aside, withholding care from unvaccinated people is also logistically unfeasible. No one I talked with could imagine a patient arriving in need and having to wait while a health-care worker checks their vaccine card. But if the hospital crisis gets worse, the urge to conserve resources may force health-care workers to make tough choices. Vaccinated patients are more likely to survive a coronavirus infection than unvaccinated ones, and health-care workers might give them more attention as a medical judgment rather than a moral one. (But such calculus is tricky: “You should preferentially give monoclonal antibodies to unvaccinated people,” Wynia told me, because each dose will be more likely to keep someone out of the hospital.)
In many cases there are good or at least understandable reasons why someone might be unvaccinated, Yong went on to say. Many poorer people say in surveys they want to get their shots or are open to the idea but can’t find time off work or away from child care, or they can’t find a provider nearby. Even the hardcore ideological refuseniks can be thought of as victims, poisoned intellectually by bad information and the grifters who peddle it. How do you separate the “deserving” unvaccinated from the “undeserving”?
The logic of Stern’s policy would also probably spill over into other medical conditions. Even if doctors continued to treat, say, lung cancer patients who’ve smoked for 40 years, the smokers themselves may incorrectly assume that they wouldn’t be treated at the hospital if they sought help because they’re to “blame” for their condition. So they’d stay home and suffer, letting a disease progress that might have been curable if they’d gone to the ER.
Stern’s solution to a problem of overstressed hospitals is draconian and unworkable but the problem does exist. A few days ago the WSJ reported that some patients in rural areas are being forced to drive hours to find an ER that can take them. That’s not because doctors are turning the unvaccinated away, it’s because the combination of surging patient loads and depleted hospital workers sidelined by Omicron means they can’t staff beds:
One or two missing workers can shut down an entire clinic. Now many are out sick with Omicron. Many rural facilities say they can’t afford to hire travel nurses at rates that have skyrocketed during the pandemic. And some clinics and family practices that typically provide care that can keep people from landing at hospitals are closing because Omicron has hobbled their workforces, too…
Sanford [Health] said hundreds of its 34,000 employees are out sick with Covid-19 and hundreds more are awaiting test results. One of the system’s critical-access hospitals has closed after all four of its nurses went out sick with Covid-19. Some patients are driving two or three hours to the nearest ER as a result. Sanford is considering cutting nonessential services and elective surgeries. It has asked asymptomatic and Covid-19-positive employees who no longer feel sick to return to work after five days.
“This is an urgent situation,” said Erica DeBoer, Sanford’s chief nursing officer.
The U.S. as a whole is on the brink of recording 2,000 daily deaths from COVID again, a number we’ve hardly seen in the past 11 months. Only for a week or so in September, at the height of the Delta wave, did it get that bad.
That’s a bummer to end on, though, so go read these optimistic pieces that things will be better — maybe even a lot better — after Omicron recedes. Some experts believe it’ll be the final wave of the pandemic. We’ve heard that before, like last spring after the vaccines were rolling out in big numbers, but an enormous majority of the population will have some form of immunity by the time Omicron’s done with us. At some point, there’s just no forest left for a fire to burn.