As cities begin to think about shutting down schools or limiting some public gatherings to prevent the spread of the coronavirus, it’s obvious to most that tens of thousands of homeless people living on the streets are at risk. Cities like Seattle, Portland and San Francisco are said to be bracing for what could come next, but how do you keep people who live outdoors in adjacent tents with no running water from getting sick?
Ann Martinez lay on a cot on the patch of grass in San Francisco where she’d be pitching her tent in a few hours, and pointed at her pals nearby. They were talking about the coronavirus crisis. The talk was a mixture of bravado, fear and resignation.
“They tell us all we’re supposed to wash our hands all the time and stay clean, but listen — we’re homeless,” she said. “How are we supposed to do that out here? And look at us. They say people are more vulnerable if we have a condition. Well, I’ve got diabetes. Some of my friends have HIV. Others have hepatitis C.
“I’m scared and I don’t know what to do.”
The city has been handing out extra hand-sanitizer for about a week but that seems like a band-aid. The real problem is that the chronic homeless, the ones who live on the streets, often have health issues that are worse than most people their age:
“If you are older and experiencing chronic homelessness, it’s more serious,” said Dr. Margot Kushel, director of the Benioff Homeless and Housing Initiative at UCSF. The frailties and ailments of chronically homeless people in their 50s or 60s resemble those of housed people about 20 years older, she said, “so this population is more vulnerable in some ways.”
The situation might be slightly better for people living in RVs because they are somewhat isolated and can move away if people living nearby get sick. But the potential for the disease to spread inside shelters, where the homeless are often sleeping close together, seems obvious.
Every night at St. Martin de Porres shelter, 212 men over the age of 50 pack in to sleep on mats on the ground 6 inches apart. Many clients here have underlying medical conditions like Smith’s, and during the day the shelter serves as a kind of medical respite for people who have nowhere else where they can go and recuperate…
…shelters are a “fertile ground” for transmission of infections like COVID-19, according to Dr. Stephen Hwang, a researcher on homelessness and health at the University of Toronto. Shelters like St. Martin de Porres could be even more susceptible than places like the Life Care Center, a long-term care facility that has been the epicenter of the COVID-19 crisis in Washington.
“People clustered together in potentially crowded indoor facilities,” Hwang said. Shelters are “sites where infection can spread quite rapidly, as they can in other settings like nursing homes.”…
St. Martin de Porres is taking steps to stop any spread of germs, cleaning surfaces with a bleach solution every two hours, and providing face masks to anyone with a persistent cough. Coronavirus fact-sheets are plastered on every wall. Staff are prepared to isolate stayers if need be: In December, when several men at St. Martin de Porres caught the flu, the T.V. room was designated as a “flu room” and infected people slept in there.
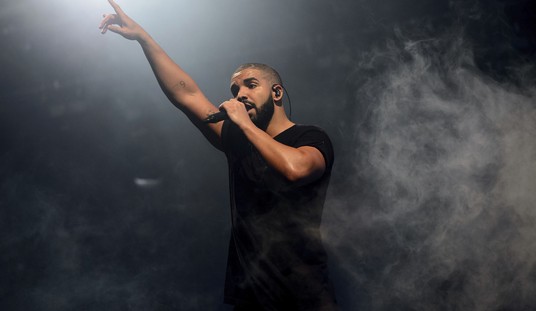
It’s good they are making a sincere effort but here’s a photo of what the sleeping arrangements look like at St. Martin de Porres. I don’t see how giving out masks to people who are already sick is going to work:

Portland is keeping two winter shelters open expecting that more people than normal will be trying to get off the streets and away from the spread of the virus:
Multnomah County officials say people diagnosed with COVID-19 won’t be staying at the two shelters. But they expect to shelter people fleeing camps where the virus may spread, as well as people with symptoms.
“We want to maintain our year-round bed capacity,” said Denis Theriault, a spokesman for the city-county joint office of homeless services. “People with respiratory symptoms may be in our shelters. No one with a confirmed COVID diagnosis will be in our shelters.”…
Anyone who’s coughing in the shelters needs to wear a mask, according to county health guidelines, and there will be at least six feet between the beds of those who are coughing or have other symptoms of illness, and those who do not. If someone tests positive for COVID-19, they will be quarantined elsewhere.
Six feet apart is a lot better than six inches but what if people are sick but not yet showing symptoms?
I wish I had some better plan to offer but, at a minimum, health workers ought to be testing everyone who comes into these facilities, especially those coming from areas where other people were showing signs of illness. That way the sick can be quickly identified and removed for treatment before they infect others who are liable to be especially vulnerable to the virus.
It’s worth saying that the danger here isn’t that the homeless will infect people who aren’t homeless. Most people don’t spend time at homeless camps or shelters where this could spread. The danger is that a lot of people could become seriously ill in a short period of time. That would obviously be bad for those people, some of whom could die as a result because they are more likely to have underlying conditions, but it also has the potential to create a strain on the medical system if it spreads quickly. That’s what all the moves toward “social distancing” are trying to avoid, but those rules are a lot harder to maintain with the homeless.







Join the conversation as a VIP Member