How could this have happened? Simply put, there’s a difference between “hospitalized with COVID-19″ and “hospitalized because of COVID-19.” Two new studies conclude that as many as 40% of all pediatric hospitalizations chalked up as severe cases of COVID-19 might not have had anything to do with the pandemic after all, NY Magazine reports this morning:
The reported number of COVID-19 hospitalizations, one of the primary metrics for tracking the severity of the coronavirus pandemic, was grossly inflated for children in California hospitals, two research papers published Wednesday concluded. The papers, both published in the journal Hospital Pediatrics, found that pediatric hospitalizations for COVID-19 were overcounted by at least 40 percent, carrying potential implications for nationwide figures.
Dr. Monica Gandhi, an infectious-diseases specialist at the University of California, San Francisco, and Amy Beck, an associate professor of pediatrics, also at UCSF, wrote a commentary for Hospital Pediatrics that accompanied the two studies. They wrote, “Taken together, these studies underscore the importance of clearly distinguishing between children hospitalized with SARS-CoV-2 found on universal testing versus those hospitalized for COVID-19 disease.” The studies demonstrate, they said, that reported hospitalization rates “greatly overestimate the true burden of COVID-19 disease in children.” Gandhi told Intelligencer that while the studies were both conducted with data from California hospitals, “there is no reason to think these findings would be exclusive to California. This sort of retrospective chart review will likely reveal the same findings across the country.”
The implications of the findings of these two studies are enormously important, as reports of pediatric hospitalizations have regularly made headlines over the past year, greatly affecting public perceptions about risks to children. Untold numbers of parents have kept children home from school or limited playdates and other activities out of fear their children would be infected and fall seriously ill. The hospitalization numbers for children were already extremely low relative to adults — at the pandemic’s peak this winter, it was roughly ten times lower than for 18-to-49-year-olds and 77 times lower than those age 65 and up. But cutting the pediatric numbers by nearly half is a striking difference, making the actual rates vanishingly small.
One can understand why the distinction might not have been made at first in the pandemic. For one thing, we didn’t entirely know whether children were vectors for the disease, but perhaps more importantly, we didn’t yet know all of the ways in which the virus attacks the body. A correlation between a SARS-CoV-2 infection and whatever the actual acute condition that required hospitalization could have been causative rather than just correlative.
That should have ended several months ago, if not perhaps even before last summer. It didn’t take that long to identify the acute symptoms of a serious COVID-19 infection, even among children, whose hospitalization rate was still far below that of adults even with the gross overstatement. The failure to correct that impression had real-world impacts on public and personal policy and behavior, much of which harmed children unnecessarily:
“It is critical that the risks of COVID-19 to children be portrayed accurately,” Gandhi and Beck wrote. “Scientific and media reports that inaccurately portray the risk of COVID-19 to children can do harm by alarming parents and providing justification for ongoing restrictions to in-person education and other programming. Via these studies, parents and policy-makers should be reassured that pediatric hospitalization for severe COVID-19 disease is indeed rare.”
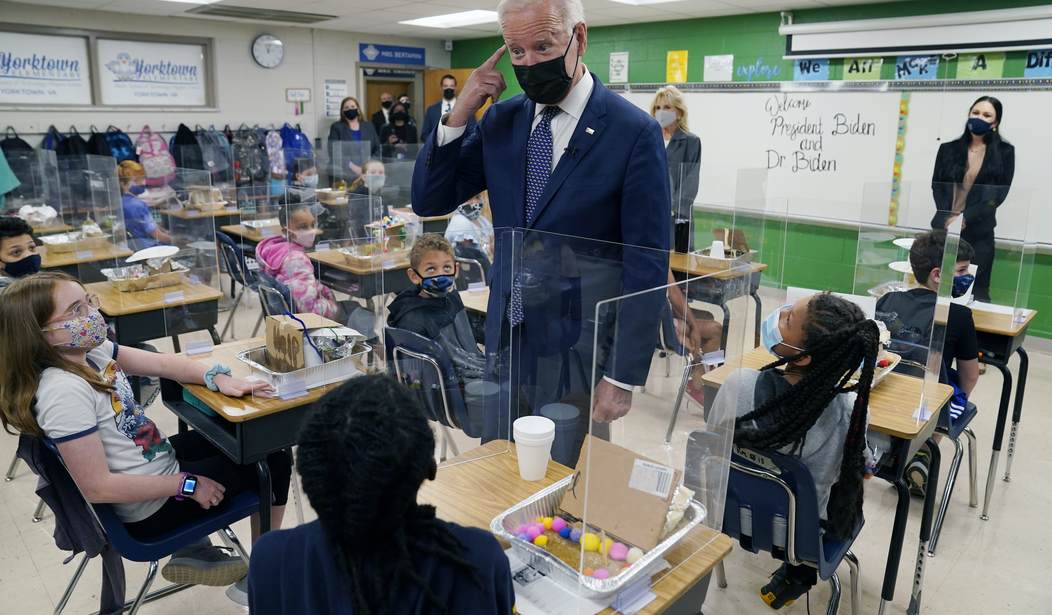
For instance, teachers unions used this data as part of its argument that in-person education presented a threat to its members. Some are now going as far as insisting that public schools remain closed until all children are vaccinated, which won’t happen until 2022 at the earliest. And this study also shows that children may not need to be vaccinated at all, or at least that parents might need to think through a risk analysis that doesn’t apply to much-more-vulnerable adults:
Stefan Baral, an infectious-diseases epidemiologist and physician at Johns Hopkins, wrote in the British Medical Journal about the risk-benefit calculus of vaccinating children against a disease that poses a “very low likelihood of severe outcomes” to them, which, he argued, means it does not meet the definition of an “emergency.” These studies weigh the scales even further toward that conclusion. The findings, Baral told Intelligencer, “reinforce the importance of going through a meaningful process to understand the risks to children.”
So far the risks of the vaccine are incredibly low too, so it makes sense in most cases to add it to a child’s vaccination schedule. However, it’s not critical in terms of pandemic containment or personal risk greater than that of the flu for this age cohort.
Finally, one has to wonder how much the correlation-not-causation issue applies to adults. Neither of the studies pursued that issue, but both researchers warn that such studies will be necessary, and soon.







Join the conversation as a VIP Member