In my experience, nutrition research is junk science.
The same is true in your own experience, I am certain. Since I am turning 60 this year, I have been given so much contradictory advice on nutrition that if I still took it seriously my head would explode.
These days I read it and get that little jolt of excitement when it tells me what I want to hear, and I dismiss it when it tells me something inconvenient. I occasionally follow the advice, but at some point trail off because, well, who knows if it is any good and changing my habits is tough.
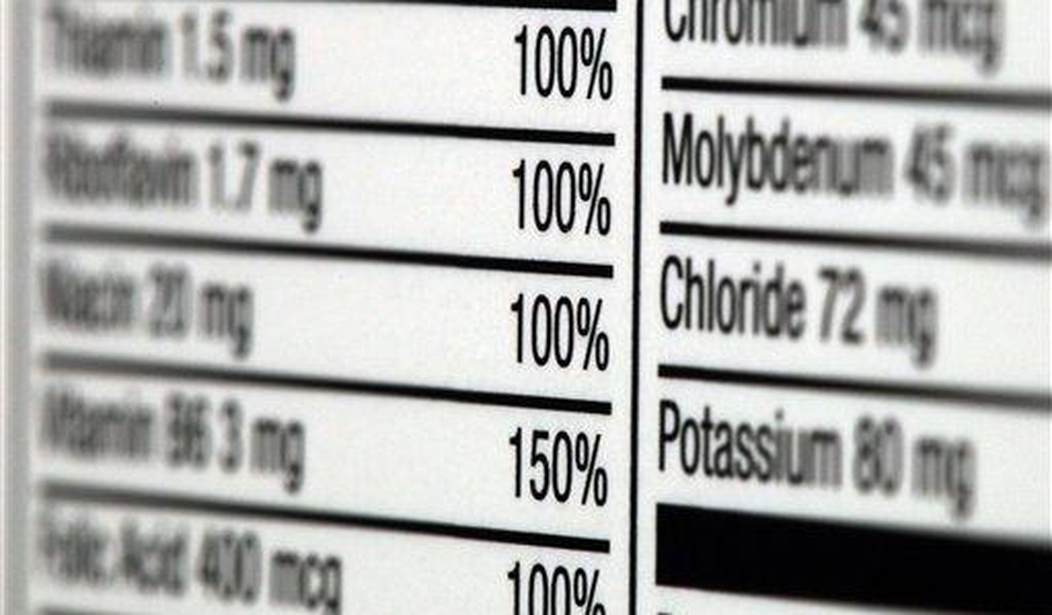
The latest bit of advice that hit the newswires is the discovery that too much niacin--a B vitamin that is used to supplement all sorts of foods, is found in B-vitamin supplements, and has been used at prescription levels to reduce cholesterol in heart patients--may cause or exacerbate heart disease.
If true, then, OOPS.
Niacin, the B vitamin that was previously used to improve lipid profile and reduce the risk of heart disease, promotes arterial inflammation and cardiovascular risk through its metaboliteshttps://t.co/ZZw51MgO0y@NatureMedicine pic.twitter.com/vSjqzgprXd
— Eric Topol (@EricTopol) February 19, 2024
Unlike most nutrition research, which is based entirely on retrospective studies with extraordinarily poor-quality evidence, this one has some oomph. And because it does, it puts more than a small dent in all that other nutrition research and even medical practice that has treated niacin as almost a wonder drug.
I have been prescribed high-dose niacin in the past to lower my cholesterol. Luckily I couldn't tolerate it and discontinued it.
The abstract of the study is typically dense and filled with lots of difficult to understand technical mumbo-jumbo, but the bottom line is clear enough: when the body metabolizes niacin it produces a by-product that is quite harmful to your blood vessels.
Despite intensive preventive cardiovascular disease (CVD) efforts, substantial residual CVD risk remains even for individuals receiving all guideline-recommended interventions. Niacin is an essential micronutrient fortified in food staples, but its role in CVD is not well understood. In this study, untargeted metabolomics analysis of fasting plasma from stable cardiac patients in a prospective discovery cohort (n = 1,162 total, n = 422 females) suggested that niacin metabolism was associated with incident major adverse cardiovascular events (MACE). Serum levels of the terminal metabolites of excess niacin, N1-methyl-2-pyridone-5-carboxamide (2PY) and N1-methyl-4-pyridone-3-carboxamide (4PY), were associated with increased 3-year MACE risk in two validation cohorts (US n = 2,331 total, n = 774 females; European n = 832 total, n = 249 females) (adjusted hazard ratio (HR) (95% confidence interval) for 2PY: 1.64 (1.10–2.42) and 2.02 (1.29–3.18), respectively; for 4PY: 1.89 (1.26–2.84) and 1.99 (1.26–3.14), respectively). Phenome-wide association analysis of the genetic variant rs10496731, which was significantly associated with both 2PY and 4PY levels, revealed an association of this variant with levels of soluble vascular adhesion molecule 1 (sVCAM-1). Further meta-analysis confirmed association of rs10496731 with sVCAM-1 (n = 106,000 total, n = 53,075 females, P = 3.6 × 10−18). Moreover, sVCAM-1 levels were significantly correlated with both 2PY and 4PY in a validation cohort (n = 974 total, n = 333 females) (2PY: rho = 0.13, P = 7.7 × 10−5; 4PY: rho = 0.18, P = 1.1 × 10−8). Lastly, treatment with physiological levels of 4PY, but not its structural isomer 2PY, induced expression of VCAM-1 and leukocyte adherence to vascular endothelium in mice. Collectively, these results indicate that the terminal breakdown products of excess niacin, 2PY and 4PY, are both associated with residual CVD risk. They also suggest an inflammation-dependent mechanism underlying the clinical association between 4PY and MACE.
You do not want major adverse cardiovascular events (MACE). Trust me.
A lot of countries mandate the fortification of foods with niacin because insufficient amounts of it cause disease. As with many nutrients, too little can cause serious problems, which is what we mean when we call something a vitamin.
Vitamins are organic molecules (or a set of closely related molecules called vitamers) that are essential to an organism in small quantities for proper metabolic function. Essential nutrients cannot be synthesized in the organism in sufficient quantities for survival, and therefore must be obtained through the diet. For example, vitamin C can be synthesized by some species but not by others; it is not considered a vitamin in the first instance but is in the second. Most vitamins are not single molecules, but groups of related molecules called vitamers. For example, there are eight vitamers of vitamin E: four tocopherols and four tocotrienols.
The term vitamin does not include the three other groups of essential nutrients: minerals, essential fatty acids, and essential amino acids.[2]
It is a matter of controversy how much of any vitamin is optimal, and of some dispute how much can be too much in many cases.
Life is complicated like that.
The reason why I am bringing all this up has little to do with this article in Nature and everything to do with just how poor the quality of science is on issues such as this.
We tend to think of physics as the model science, and even in physics, the lines can get blurry on how well we really understand a lof of things. Still, in physics, we have done a pretty good job of following good scientific methods and developing a strong knowledge base on most of the major issues. The open questions are huge, and our paradigms are hardly perfect, but when I read physics papers, I am generally confident that the scientists aren't blowing smoke.
That's not really true in many of the other sciences, where there is a lot of confident hand-waiving and smoke-blowing, and much less solid knowledge and good-quality research being done. This is especially true in studying highly complex systems where it is literally impossible to do what we normally do in physics: isolate various components of a problem and build from the ground up a simplified model that tells us important things.
Biological, sociological, and psychological systems are all highly interdependent and complex, where isolating one variable may disturb the entire balance of a system. So much of what we read is based on poor-quality data, improper methods, or the result of fishing expeditions that can produce spurious results.
So, what do I think about this particular study? It sounds interesting, and at least it shows a clear mechanism for what they have found. They don't appear to be blowing smoke or handwaving, so that is good. As for it being right, we shall see if it gets replicated.
But if it does turn out to be right, consider what that means: for decades, doctors and regulators have been harming people based on bad science, of which there is so much.
How many of you out there have quaffed massive quantities of niacin based on potentially awful advice? More than a few, I imagine. I did for a bit, and for all I know, I am getting too much from the B vitamins I take every morning.
Dr Prasad is almost certainly right: the best path is to follow your grandmother's nutrition advice.







Join the conversation as a VIP Member